|
|
|
Rationale and preliminary results of endovascular treatment of multiple sclerosis,
the liberation procedure
P Zamboni, R Galeotti, E Menegatti, AM Malagoni, F Mascoli, S Dall-Ara, I Bartolomei,
F Salvi
Introduction
Multiple sclerosis is an inflammatory, demyelinating disease of the central nervous
system of unknown pathogenesis; it is considered to be autoimmune in nature.[1][2]
It is the most common disease causing disability in young people. The clinical course
is usually classified as relapsing remitting (characterized by acute exacerbations
of the disease followed by complete or partial recovery), secondary progressive
(characterized by progressive deterioration of neurologic function after several
years of relapsing remitting course), and primary progressive (characterized
by a progressive clinical course starting from the beginning).[3]
Magnetic resonance venography[4-7] and post mortem studies [8] demonstrated a topographic
correspondence between multiple sclerosis plaques and the cerebral venous system.
Histologic examination of the involved veins reveals unequivocally the presence
of characteristic signs of impaired venous drainage, such as perivenous iron deposits
and fibrin cuffs, particular to chronic venous insufficiency.[9]
All of these elements convinced the current authors to investigate Doppler cerebral
venous hemodynamics.[10] Cerebrospinal venous return in multiple sclerosis patients
was found to be anomalous with respect to controls (including healthy subjects matched
for age and gender, patients affected by other neurologic diseases, and healthy
subjects older than the median age of onset of multiple sclerosis). [11-13] Venous
hemodynamics was investigated by combining extracranial echo-colour-Doppler of the
internal jugular veins colour-Doppler sonography was used for studying the deep
cerebral veins, focusing on the detection of five anomalous parameters, which are
absent in normal subjects (Table 1)[10]
Sensitivity, specificity, positive predictive value and negative predictive value
were tested for significance by the two-sided Fisher exact test, by comparing the
gold standard diagnostic assessment, represented by clinical and magnetic resonance
Imaging revised McDonald criteria for diagnosis of multiple sclerosis, with the
proposed echo-colour-Doppler-trans-cranial colour-Doppler sonography protocol.
Table 1. Echo-colour-Doppler-trans-cranial colour-Doppler sonography parameters
of abnormal
cerebral venous outflow in multiple sclerosis
|
|
Echo-colour-Doppler-
trans-cranial colour-
Doppler sonography
parameters
|
Multiple
sclerosis (%) |
Control
populations (%)
|
Sensitivity Specificity
Positive predictive value-
Negative predictive value
(95% Cl)
|
p |
|
1. Spontaneousreflux
constantly present in the
internal jugular veins and\
or vertebral veins in both
sitting and supine posture |
70% |
0% |
100%(95-100)
84% (79-89)
70% (60-78)
100% (98-100) |
<0.0001 |
2. Reflux propagated
upward to the deep
cerebral veins |
50%/o |
0% |
100% (93-100)
77% (71-82)
50% (41-60)
100% (98-100) |
<0.0001 |
3. High resolution Bmode
evidence of proximal
internal jugular vein
stenosies |
28% |
0.6% |
97% (83-99)
69% (63-75)
28% (19-37)
99% (97-100) |
<0.0001
|
4. Flow not Doppler
detectable in the
internal jugular veins
and/or vertebral veins
despite numerous deep
inspirations |
32% |
0.6% |
97% (85-99)
70% (64-76)
32% (23-42)
99% (97-100) |
<0.0001 |
5. IJV cross-scctional
area in sitting posture
> than in supine posture |
58%
|
12%
|
74% (63-83)
76% (70-82)
56% (46-65)
88% (82-92) |
<0.0001 |
|
Conciusive Analysis
Two or more Echo-
colour-Doppier-trans-
cranial colour-Doppler
sonography positive
parameters |
100% |
0% |
100%
100%
100%
100%
|
<0.0001 |
Venography and 'intent to treat' procedures
Diagnosis of suspicious abnormal extraeranial cerebral venous outfiow must fulfil
at least two of the five criteria listed in Table 1 and is taken as an indication
approved by the Ethical Committee of the current authors' hospital to continue the
study using selective venography in all suspccted subjects. [12]
Selective venography demonstrates that anomalies in Doppler venous hemodynamies
are due to multiple significant extracranial venous stenosis, localized at the cervical,
thoracic, and less commonly abdominal level of the principal cerebrospinal venous
segments. In a further control population with negative ultrasound results, which
includes subjects not affected by neurologic diceases who underwent venography for
other reasons, stenotic patterns were never demonstrated in the internal jugular
veins, azygous, and lumbar territory. [12] In particular, the azygous vein in the
multiple sclerosis group was affected in 86% of cases. Most cases involved membranous
obstructions of the junction with the superior vena cava, or, less frequently, twisting,
septums and atresias as can be seen in the x-rays in Figure 1.
In 12 cases, the azygous system presented stenosies at several points up to even
atresia or agenesis of the lumbar plexuses (18%). As for the jugular veins, they
were found to be stenosed unilaterally or bilaterally in 59 out of 65 cases (91%).
The stenosies were frequently annulus (Fig. 2) and septum, followed by atresias,
and rarely by ageneses; no twisting was observed, sometimes coexistent valvular
anomalies and bone compression were also observed. Interestingly, the distribution
of the extracranial venous stenosies significantly influences the clinical course
as well as the onset of symptoms.[11]
Selective phlebography enabled the current authors to perform a first treatrnent
of the identified venous obstructive lesion at the time of the diagnostic evaluation
by the means of balloon angioplasty, the so called liberation procedure. Twisting
of the azygous vein in nonresponders has been subsequently treated by stent insertion.
Intent to treat procedures at the time of diagnostic phlebography was performed
in 77 consecutive cases. The ethical committee approved this study in February 2007.
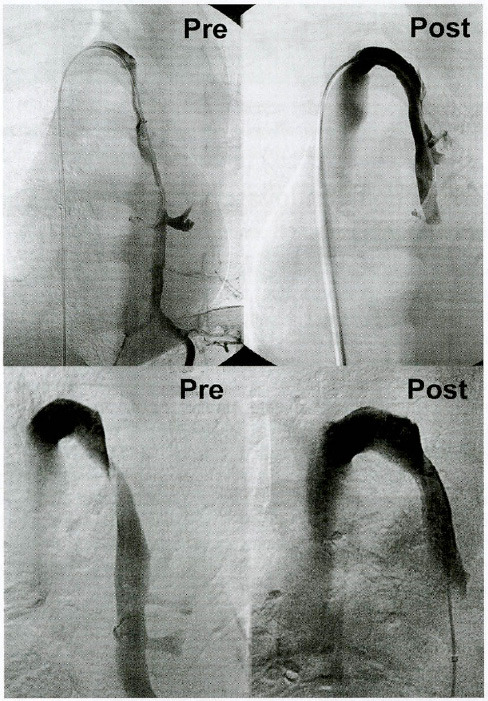
Figure 1. (Top left) Preoperative venography of the azygous vein affected
by combination of membraneous obstruction of the outlet into the superior vena cava
and proximal atresia, with reflux extended downward to the emiazygous vein. (Top
right) Postoperative result with reflux disappearance. (Bottom left) Preoperative
venography of azygous vein affected by twisting. (Bottom right) Postoperative result
after angioplasty.
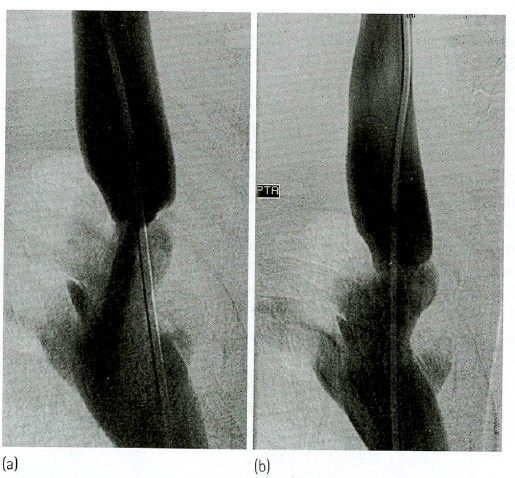
Figure 2. (a) Closed stenosis of the internal jugular vein. (b) The same
case after balloon angioplasty
Results of venous endovascular procedures in multiple sclerosis
All procedures were performed in day hospital and under local anesthesia. The procedure
was well tolerated. Post-procedural observation was carried out at 4 hours and the
patients were discharged with a compressive dressing on the left femoral vein, the
preferred site of vascular access. The dressing could be removed the day after the
procedure. A prophylactic dose of low-molecular-weight heparin is strongly recommended
for the subsequent 3 weeks.[14] No operative and postoperative complications were
registered, including vessel rupture, thrombosis, or side effects caused by the
contrast media. Minor hemorrhages with hematomas in the site of vascular access
were occasionally seen.
Patients who underwent a cerebrospinal venous endovascular procedure were followed
up by means of a validated clinical test for investigatirig the motility of upper
and lower extremities as well as the cognitive function (the so-called multiple
sclerosis functional composite MSFC), the expanded disability status scale, EDSS,
and a recognized QoL. questionnaire MSQoL-54, in addition to clinical and magnetic
resonance imaging measure)[15][16][18-20]
The venous patency and its relationship with the clinical course was also evaluated.
Clinical resuits
Acute attack in relapsing remitting patients
About 85% of multiple sclerosis cases begin with relapsing remitting disease; this
evolves through recurrent exacerbations with subscquent full or Partial recovery
before entering the progressive phase, in which any recovery of function is rare.
Relapse events average about 1.1 per year early in the disease course.[21]
Relapse in the relapsing remitting clinical course is unpredictable and clinically
manifests with the impairment of one or more neurologic functions. Acute attacks
are usually managed with high-dose corticosteroids for 5 days. Relapse is associated
with magnetic resonance imaging evidence of inflammation.
In Emergency, 18 consecutive patients were treated without use of corticosteroids,
using the endovascular techniques described earlier. A total recovery time ranging
from 4 hours to 4 days from endovascular treatment was observed. This was the best
evidence that venous obstructions play a causative role in the complex pathogenesis
of multiple scierosis. This group of patients was followed up together with the
other patients of the relapsing remitting group treated electively. Outcome measures
will be described next.
Preliminary results in relapsing remitting patients
A total of 51 patients were treated with the relapsing remitting clinical course,
18 in Emergency for acute attack as described earlier, and 33 electively. Moreover
13 and 11 patients were treated, respectively, with secondary progressive and primary
progressive clinical courses. This chapter herein refers exclusively to results
ohtained on the relapsing remitting patients. The outcorne measures are those usually
utilized in clinical trials evaluating multiple sclerosis treatment:
- Rate of relapse in the year subsequent to the endovascular procedure as compared
to the rate registered in the same population in the proceding year (Fig. 3). The
probability of acute attack decreased more than 4-fold after the endovascular treatmcnt,
OR = 4.4 (95% CI 1.5-13, p = 0.0072);
- MSFC Z-score, expressing the score of lower limb motility, plus upper limb motility,
plus cognitive performance.[15-16] It was significantly improved 1 and 6 months
postoperatively as can be casily seen in Figure 4;
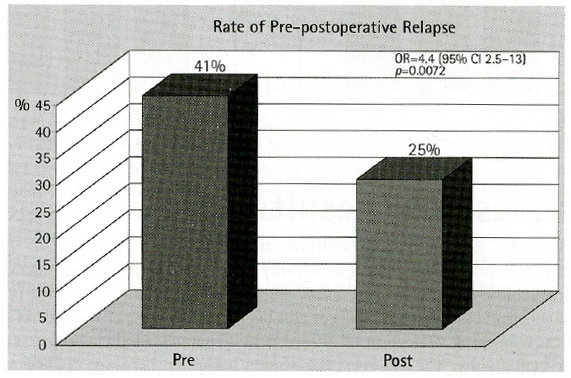
Figure 3. Significant reduction of the relapse rate n the first year after
venous balloon angioplasty.
- QoL by using a validatcd 54-item questionnaire focused on multiple sclerosis.[18]
The score was significanily increased by about 30%, as shown in Figure 5, in the
composite parts concerning physical and mental status. QoL improvement is confirmed
by the dramatic improvement registered in chronic fatigue. The latter aspect was
also measured separately, registering a reduction of 50% on the validated fatigue
scale[17] (p < 0.01). It is stressed that chronic fatigue is one of the more disabling
symptoms in multiple sclerosis, and is actually orphan of any effective treatment;
- A follow-up MRI has not been carried out.
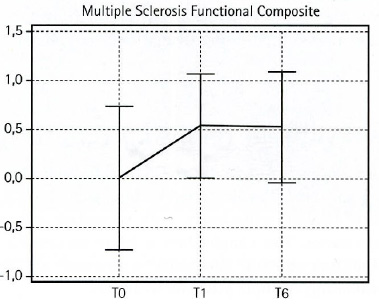
Figure 4. Z-score mean - SD of the multiple sclerosis functional composite
at baseline and after the endovascular procedure (p < 0.05).
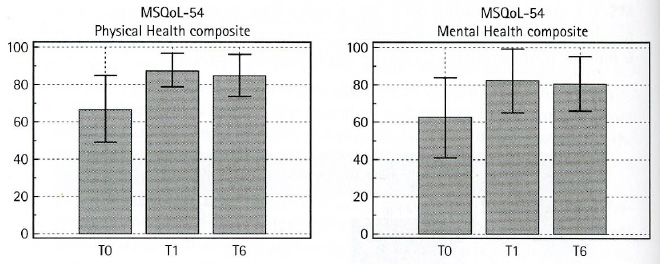
Fiqure 5. QoL improvement after the endovascular procedure (mean - SD, p
< 0.05).
Endovascular results
Post-procedural cerebral venous outflow surveillance was performed at 1, 3, and
6 months, and subscqucntly on a 6-monthly basis, by means of the detection of the
same echo-colour-Doppler-trans-cranial colour-Doppler parameters shown in Table
1. Vascular ultrasonography was additionally performed in case of clinical relapse
and/or clinical worsening. Detection of altered hemodynamics would represent an
indication for venography. The endovascular resuits presented here are divided according
to venous segment.
Procedures on azygous vein
Membranous obstruction of the outlet of the azygous vein into the superior vena
cava can be successfully managed by simple balloon dilatation. This procedure was
performed in 38 out of 77 cases, and no recurrence was recorded at 1 year. Twisting
of the azygous vein was obscrved in seven out of 77 cases that were also treated
by balloon angioplasty. The atter recurred in two cases (29%), which were subsequently
treated hy stent insertion with a 6-month patency (Fig. 6). The same anti-platelet
protocol is used in balloon angioplasty and stenting at the level of the coronary
artery, in addition to administration of low-molecularweight heparin[23].
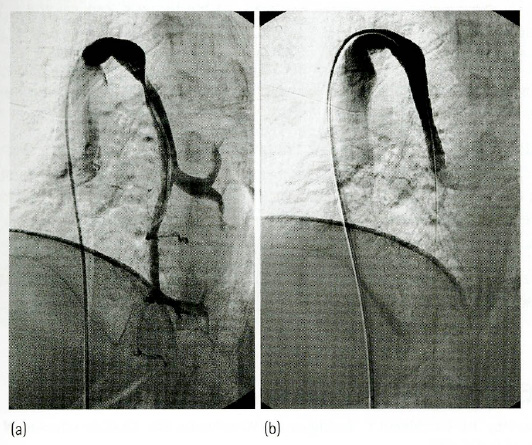
Figure 6. (a) Twisting of the azygous vein not responding to simple balloon
angioplasty, causing reflux downward and inward to the spinal cord. (b) Successful
stent insertion at the azygous arch with elimination of twisted stenosis and reflux.
Procedures on internal jugular veins
In contrast, overall internal jugular vein stenosies were present in 94 of 144 patients
and internal jugular vein patency was achieved at 1 year in 66 of 94 patients (70%).
All patients with restenosis corresponded to those who manifested relapses in the
year subsequent to the endovascular treatment (Fig. 3). Symptomatic and asymptomatic
restenosies were again treated with balloon dilatation. However, no attempt at a
stenting procedure was made in the absence of a dedicated device capable of preventing
migration. This device would fit the particular rnorphology of the internal jugular
vein, similar to a upside down milk bottle, and, finally avoid protrusion into the
brachiocephalic trunk.
Summary
- Multiple sclerosis is an infiammatory demyelinating disease of the central nervous
system of unknown pathogenesis. It is considered to be autoimmune in nature and
is the most common disease causing disability in young people.
- In multiple sclerosis the plaques are venocentric, with some histologic aspects
particular to chronic venous disease. The Doppler hemodynamics of cerebrospinal
venous return in multiple scierosis patients is consistently altered.
- Investigation of multiple sclerosis patients with Doppier anomalies of cerebral
venous return by means of venography demonstrates multiple stenosies, affecting
the principal extracranial venous segments at the thoracic, cervical and sometimes
abdominal level.
- The majority of venous stenosies are treatable at the time of venography with conventional,
minimally invasive, and safe endovascular techniques, the so called liberation procedure.
- Endovascular treatment, with the limitation of a short follow up, improves significantly
the validated outcome measure in multiple sclerosis, including the multiple sclerosis
functional compositum score and QoL assessment. In addition, It reduces by more
than four times the relapse rate in the year subsequent to the procedure, as compared
to the preceding year.
- Treatment of the azygous vein and of the jugular vein showed a 1-year patency of
95% and 70%, respectively.
References
- Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG. Multiple sclerosis. N
Engl J Med 2000; 343: 938-952.
- Frohman EM, Racke MK, Raine CS. Multiple sclerosis-the plaque and its pathogenesis.
N Engl J Mcd 2006; 354: 942-955.
- Polman CH, Reingold SC, Edan G, Filippi M, Hartung H-P. Diagnostic criteria for
multiple sclerosis: 2005 revisions to the McDonald Criteria: Ann Neurol 2005; 58:
840-846.
- Yulin GE, Vahe M, Zohrabian RI. Grossman, seven-tesla magnetic resonance imaging.
New vision of microvascular abnormalities in multiple sclerosis. Arch Neurol 2008;
65: 812-816.
- Kermode AG, Thompson AJ, Tofts P et al. Breakdown of the blood-brain barrier precedes
symptoms and other MRI signs of new lesions in multiple sclerosis. Pathogenetic
and clinical implications. Brain 1990; 113: 1477-1489.
- Kidd D, Barkhof F, McConnell R, Algra PR, Allen IV, Revesz T. Cortical lesions in
multiple sclerosis. Brain 1999; 122: 17-26.
- Tan IL., van Schijndel RA, Pouwels PJ. MR venography of multiple sclerosis. Am J
Neuroradiol 2000; 21: 1039-1042.
- Fog T. The topography of plaques in multiple sclerosis with special reference to
cerebral plaques. Acta Neurol Scand Suppl 1965; 15: 1-161.
- Zamboni P. Iron-dependent inflammation in venous disease and proposed parallels
in multiple sclerosis. J R Soc Med 2006; 99: 589-593.
- Menegatti E, Zamboni P. Doppler haemodynamics of cerebral venous return. Curr Neurovase
Res 2008; 5: 11 (in press 2009).
- Zamhoni, P, Menegatti E, Bartolornei I et al. Intracranial venous haemodynamics
in multiple sclerosis. Curr Neurovase Res 2007; 4: 252-258.
- Zamboni P, Galeotti R, Menegatti E er al. Chronic cerebrospinal venous insufficiency
in patients with multiple sclerosis. (Neurol Neurosurg Psychiatry 2008 Dec, online
first).
- Zamboni P, Galeotti R, Menegatti E. et al. Altered Doppler venous haemodynamics
in multiple sclerosis: a mechanism increasing iron stores? (In press J Neur Sci
September 2009).
- Geerts Wil, Bergqvist D, Pineo GF et al. Prevention of venous thromboembolism: American
College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition).
Chest 2008; 133(Suppl 6): 381S-453S.
- Cutter GR, Baier ML, Rudick RA et al. Development of a multiple sclerosis functional
composite as a clinical trial outcome measure. Brain 1999; 122: 871-882.
- Fisher JS, Rudick R, Cutter G, Reingold SC. The Multiple Sclerosis Functional Compositc
measure (MSFC): an integrated approach to MULTIPLE SCLEROSIS clinical outcome assessment.
Mult Scler 1999; 5: 244-250.
- Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional
impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis
1994; 18(Suppl 1): S79-S83.
- Vickrey BG, Hays RD, Harooni R, Myers LW. Ellison GW. A health-related quality of
life measure for multiple sclerosis. Qual Lfe Res 1995; 4:187-206.
- Kurtzke JF. Rating neurological impairment in multiple sclerosis: an expanded disability
scale (EDSS). Neurology 1983; 33: 1444-1452.
- Rizvi SA, Agius MA. Current approved options for treating patients with multipic
sclerosis. Neurology 2004; 63: S8-S14.
- Volimer T. The natural history of relapses in multiple sclerosis. J Neurol Sci 2007;
15: S5-S13.
- Becker RC, Meade TW, Berger PB et al. The prirnary and secondary prevention of coronary
artery disease: American College of Chest Physicians Evidence-Based Clinical Practice
Guidelines (8th edn). Chest 2008; 133: 776S-814S.
(C)2009: Front and Front2
|
|